Open Access, Volume 9
Desmoid-type fibromatosis in splenic hilum with rupture of lienal artery aneurism in a 17-year-old male
Blagica Krsteska1*; Rubens Jovanovic1; Aleksandar Eftimov1; Ljubomir Ognjenovic1; Darko Dzambaz1
1Institute of Pathology, Faculty of Medicine, Ss Cyril and Methodius University in Skopje, Republic of North Macedonia.
2Faculty of Medicine, University Clinic of Abdominal surgery, Ss Cyril and Methodius University in Skopje, Republic of North Macedonia.
Blagica Krsteska
Institute of Pathology, Faculty of Medicine, Ss Cyril and Methodius University in Skopje, Republic of North
Macedonia.
Email: blagicadr@yahoo.com
Received : February 20, 2023
Accepted : March 27, 2023
Published : March 31, 2023,
Archived : www.jclinmedcasereports.com
Abstract
Desmoid Fibromatosis (DF) is locally aggressive benign fibroblastic or myofibroblastic tumor with no metastatic potential, but has high recurrence rate. The symptoms vary according to tumor location, abdominal or extra-abdominal. In this study we present a case of a 17-year-old male with intraabdominal bleeding due to rupture of lienal artery aneurism in splenic hilum where desmoid fibromatosis was found. From abdominal cavity 3L free blood was evacuated. Immunohistochemistry revealed nuclear positivity for β-catenin stain favoring the diagnosis of desmoid type fibromatosis. Some of the cells showed SMA positivity, while CD34, S100 and CD117 were negative. Additional molecular analysis from 3 ml peripheral blood was made by NGS showing intergenic variant on position 51549496 with frequency of 46,4% which is highly pathogenic. Intraabdominal fibromatosis has very unpredictable outcome when diagnosed incidentally. Molecular analysis should reveal more genetic alterations in publishing these case presentations.
Keywords: Myofibroblastic tumor; Hemoperitoneum; β-catenin mutations.
Copy right Statement: Content published in the journal follows Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0). © Krsteska B (2023)
Journal: Open Journal of Clinical and Medical Case Reports is an international, open access, peer reviewed Journal mainly focused exclusively on the medical and clinical case reports.
Citation: Krsteska B, Jovanovic R, Eftimov A, Ognjenovic L, Dzambaz D. Desmoid-type fibromatosis in splenic hilum with rupture of lienal artery aneurism in a 17-year-old male. Open J Clin Med Case Rep. 2023; 2003.
Introduction
Desmoid Fibromatosis (DF) is locally aggressive benign fibroblastic or myofibroblastic tumor with no metastatic potential, but has high recurrence rate. It is a rare disease accounting 3% of all soft tissue tumors. There are reported two relatively peaks of the disease occurrence: one between 6-15 years and one between puberty and 40. The symptoms vary according to tumor location. Abdominal DF occurs in the mesentery, abdominal wall, hilar regions, previous surgical sites. Extra abdominal DF is deeply seated in the soft tissues on extremities or head and neck. The biologic behavior is unpredictable and variable. The etiology is unknown, but may be associated with previous trauma or as a feature in Gardner’s syndrome or Familial Adenomatous Polyposis (FAP).
Depending of the local invasion, deep muscles, fascia, vascular branches, complete surgery is often difficult to achieve. Recurrence of DF is hard to predict, but in most cases depends of quality of surgery and radiation therapy. New biological and target therapies are emerging due to tumor biology and molecular pathways [1].
Case Presentation
A 17-year-old male presented symptoms of collapse with intense abdominal pain and he was brought by his parents to the Emergency Department in University Clinic Mother Teresa in Skopje. Hypovolemic shock was diagnosed and CT finding of free blood in abdominal cavity with ruptured aneurysmal dilatation of lienal artery near the splenic hilum. After short reanimation he underwent surgical treatment and splenectomy was performed at University Clinic of Abdominal surgery. From abdominal cavity 3 L free blood was evacuated. The postoperative period went well and the patient was dismissed in good condition
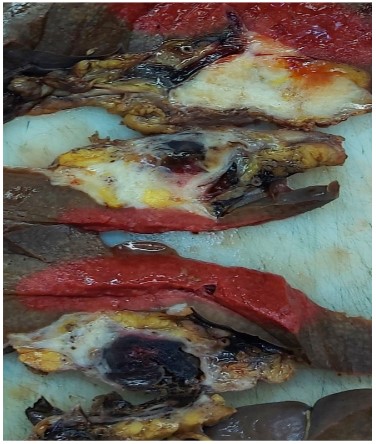
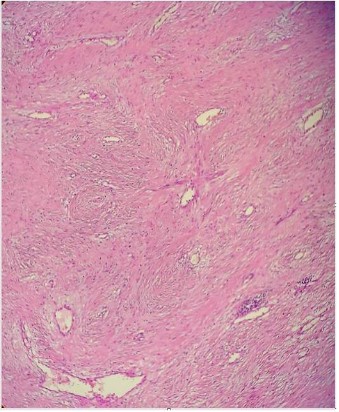
The operative material was analyzed at Institute of pathology, Faculty of Medicine in Skopje. The spleen was 277 g in weight and measured 10,5 x 9 x 4,5 cm. Gross examination of the cut sections at the splenic hilum showed solid white tissue with infiltrative borders measuring 4 x 3 x 2,5 cm. Near this tumor mass there was aneurismal dilatation of splenic artery with intraluminal clot and wall perforation (Figure 1a). Tissue specimens were fixed in formalin, embedded in paraffin and stained with hematoxylin & eosin.
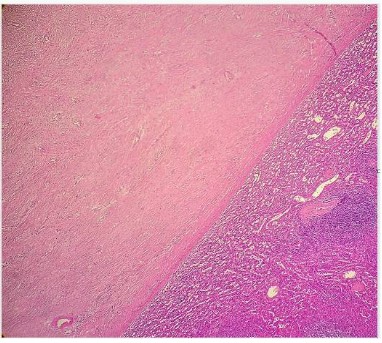
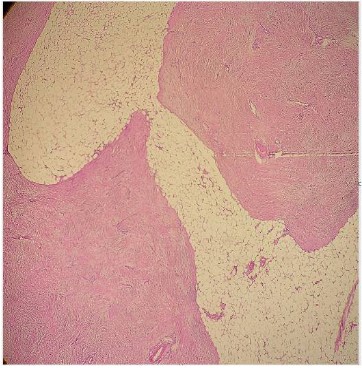
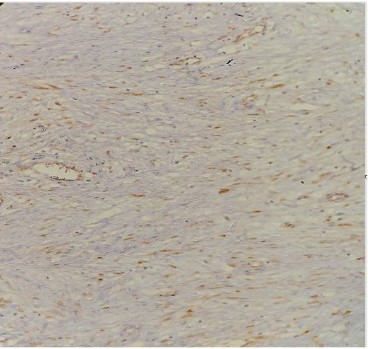
Microscopic analysis revealed myofibroblastic proliferation with infiltrative borders near to spleen capsule, without parenchymal involvement (Figure 1b, 1c). On higher magnification there were uniform, elongated, spindle cells with fascicle arrangement and thin-walled blood vessels with perivascular edema (Figure 1d). No nuclear atypia or mitoses were found. Immunohistochemistry revealed nuclear positivity for β-catenin stain favoring the diagnosis of desmoid type fibromatosis (Figure 1e). Some of the cells showed SMA positivity, while CD34, S100 and CD117 were negative. Proliferative marker Ki67 was low.
Additional molecular analysis from 3 ml peripheral blood was made by Next Generation Sequencing. The results showed intergenic variant on position 51549496 with frequency of 46,4% which is highly pathogenic, intergenic variant on position 151948366 with frequency of 100% with unknown clinical significance, and following mutations: c.3961G>A p.(Val1321Ile) in BLM gene, c.221A>C p.(Asp74Ala) in CDK2A gene, c.1544A>G p.(Lys515Arg) in PALB2 gene and c.25A>G p.(Thr9Ala) in WRN gene.
Discussion
Desmoid fibromatosis is rare benign fibroblastic tumor with infiltrative borders and variable unpredictable clinical course. It may be associated with FAP (Familial adenomatous polyposis) in 5-10%, but usually occurs sporadically. Meyer et al. talk about rare sporadic pancreatic desmoid fibromatosis in patient with history of colon adenocarcinoma and renal cell carcinoma [1]. DF occurs at previous surgical resection sites, especially when intra-abdominal, after cholecystectomy or colectomy for carcinoma, sarcoma or FAP [2-6]. Our patient didn’t have any previous surgical intervention.
Tatsumi et al. present a case of splenic artery aneurysm invaded by DF causing death of the patient [7]. The case that we present has successful treatment after rupture of splenic artery aneurysm. The splenic hilum is unusual location for DF, in literature reported in elderly patient with previous nephrectomy for renal cell carcinoma and in a middle-aged woman mimicking gastrointestinal stromal tumor affecting pancreatic tale and gastric lesser curvature [8,9]. Abdominal desmoid tumors can be superficial and intrabdominal. Intraabdominal desmoid tumors can surround vessels and organs, thereby complicating their function and hence surgical treatment [10].
Morphological patterns include: conventional, hypocellular/hyalinized, staghorn vessels, myxoid, keloidal, nodular fasciitis-like and hypercellular type. In a study of 165 serial cases the morphological pattern was correlated by site and sex [11]. Intraabdominal DF showed the greatest morphological variability and female predominance. This study didn’t find significant correlation between the histologic type and clinical outcome in the meaning of recurrence and FAP/Gardner syndrome [11].
In differential diagnosis scar formation, Solitary Fibrous Tumor (SFT), synovial sarcoma, inflammatory myofibroblastic tumor and Gastrointestinal Stromal Tumor (GIST) must be excluded by immunohistochemistry or genetic analysis. CD117 or DOG-1 reactivity will favor the diagnosis of GIST, and b-catenin positive nuclear stain will confirm DF. SFT has staghorn vessel network and immunohistochemically is CD34 and STAT6 positive [11]. Inflammatory myofibroblastic tumor is characterized by rich inflammatory component by lymphocytes, plasma cells and eosinophils with myofibroblastic proliferation.
In a study of 59 pediatric cases with DF, thirty-eight developed one or more recurrences and disease progression [12]. Intra-abdominal desmoid fibromatosis, although rare in pediatric patients was presented in a yang male in ileo-colic region with mass effect requiring surgical intervention [13]. Head and neck regions are seen in 7-15% of all DF and more than half are in children. The youngest patient with largest DF is presented with parapharyngeal tumor [14]. Acute abdomen is a condition when DF is initially diagnosed due to complications [15]. Negative margin status is important for the prognosis of abdominal cases of desmoid fibromatosis after surgery [16].
Colombo et al. in their study of 33 cases of DF demonstrated two distinct molecular subgroups regarding β-catenin stability, α-catenin affinity and gene expression profiling, one carrying T41A or S45F mutations, and one that is WT (wild type) β-catenin [17]. In pediatric patients the molecular analysis may harbor broader mutational spectrum [18].
Conclusion
Intraabdominal fibromatosis has very unpredictable outcome when diagnosed incidentally. Molecular analysis should reveal more genetic alterations in publishing these case presentations or bigger case studies. DF should be included in differential diagnosis in patients with intraabdominal bleeding or acute abdomen.
Declarations
Consent form: Informed consent was obtained from the patient.
Conflict of interest: The authors declare no conflict of interest.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Mastoraki A, Schizas D, Vassiliu S, Saliaris K, Giagkos GC, et al. Evaluation of diagnostic algorithm and therapeutic interventions for intra-abdominal desmoid tumors. Surg Oncol. 2022; 41: 101724.
- Meyer A, Szajnbok P, Koszka AJM, Pezzutti D, Segatelli V, et al. A rare sporadic pancreatic desmoid fibromatosis with splenic vein invasion diagnosed by CT scan-guided core needle biopsy: a case report with possible differential diagnosis from metastatic colorectal or renal cancer. J Surg Case Rep. 2021; 2021: rjab257.
- Damiani G, Mikhael R, Tzanis D, El Zein S, Bonvalot S. Desmoid Tumors Arising on the Mesenteric Surgical Scar of Abdominal Sarcomas. Cureus. 2022; 14: e21727.
- Rangunwala J, Sitta J, Prakash V, Vyas K, Roda M. Complex Case of Aggressive Intra-abdominal Desmoid-type Fibromatosis Status Post Cholecystectomy. Cureus. 2020; 12: e7193.
- Terada I, Hashimoto M, Zaimoku R, Takei R, Terakawa H, et al. A Case of Intra-Abdominal Desmoid Tumor after Laparoscopic Resection of Colon Cancer. Gan To Kagaku Ryoho. 2022; 49: 217-219.
- Vitellaro M, Sala P, Signoroni S, Radice P, Fortuzzi S, et al. Risk of desmoid tumours after open and laparoscopic colectomy in patients with familial adenomatous polyposis. Br J Surg. 2014; 101: 558-565.
- Tatsumi K, Bundock EA. Splenic Artery Aneurysm Invaded by Desmoid-Type Fibromatosis. Am J Forensic Med Pathol. 2015; 36: 202-204.
- Sanchez-Gollarte A, Mendoza-Moreno F, Perez-Gonzalez M, Diez-Alonso M, Muguerza-Huguet JM, et al. Desmoid-type Fibromatosis of the Splenic Hilum: A Rare Tumor at an Unusual Location. Niger J Surg. 2020; 26: 166-169.
- Kotidis E, Strati TM, Triantafyllou E, Ioannidis O, Pramateftakis MG, et al. Laparoscopic Resection of Desmoid Type Fibromatosis of the Splenic Hilum Mimicking a Greater Curvature Gastric GIST. J Coll Physicians Surg Pak. 2018; 28: 714-716.
- Sakorafas GH, Nissotakis C, Peros G. Abdominal desmoid tumors. Surg Oncol. 2007; 16: 131-142.
- Zreik RT, Fritchie KJ. Morphologic Spectrum of Desmoid-Type Fibromatosis. Am J Clin Pathol. 2016; 145: 332-340.
- Oudot C, Orbach D, Minard-Colin V, Michon J, Mary P, Glorion C, et al. Desmoid fibromatosis in pediatric patients: management based on a retrospective analysis of 59 patients and a review of the literature. Sarcoma. 2012; 2012: 475202.
- Zheng Z, Jordan AC, Hackett AM, Chai RL. Pediatric desmoid fibromatosis of the parapharyngeal space: A case report and review of literature. Am J Otolaryngol. 2016; 37: 372-375.
- Sioda NA, Wakim AA, Wong T, Patel S, Coan K, Row D. A Large Sporadic Intra-abdominal Desmoid-Type Fibromatosis in a Young Male: A Case Report. Front Surg. 2020; 7: 60.
- Morris D, Gonzalez R, Cook J, Metts J, Shaw P. Gastrointestinal Complications of Intra-Abdominal Desmoid Tumors: A Case Report and Review of the Literature. Case Rep Oncol. 2022; 15: 515-521.
- Zheng Q, Liu B, Zhou Y, Liu D. Prognostic factors of abdominal desmoid tumor after surgery: A retrospective study of 52 patients. Asian J Surg. 2022; 45: 1770-1771.
- Colombo C, Belfiore A, Paielli N, De Cecco L, Canevari S, Laurini E, et al. beta-Catenin in desmoid-type fibromatosis: deep insights into the role of T41A and S45F mutations on protein structure and gene expression. Mol Oncol. 2017; 11: 1495-1507.
- Trautmann M, Rehkamper J, Gevensleben H, Becker J, Wardelmann E, Hartmann W, et al. Novel pathogenic alterations in pediatric and adult desmoid-type fibromatosis - A systematic analysis of 204 cases. Sci Rep. 2020; 10: 3368.