Open Access, Volume 9
Rat bite fever with multifocal musculoskeletal infection and septic shock
Clara Batista1; Susana Ramos Oliveira1; Sofia Jordão1; João Carlos Rodrigues2; Carlos Abel3; R. Correia de Abreu1; Isabel Neves1
1Department of Infectious Diseases, Pedro Hispano Hospital - Local Health Unit of Matosinhos, Matosinhos, Portugal.
2National Health Institute Doutor Ricardo Jorge (INSA), Infectious Diseases Department, Lisboa, Portugal.
3Department of Radiology, Pedro Hispano Hospital - Local Health Unit of Matosinhos, Matosinhos, Portugal.
Clara Batista
Pedro Hispano Hospital, Local Health Unit of Matosinhos, Matosinhos, Portugal.
Email: clara_bbatista@hotmail.com
Received : Received: Dec 15, 2022,
Accepted : January 26, 2023
Published : January 31, 2023,
Archived : www.jclinmedcasereports.com
Abstract
We report an unusual, severe and transient skin color changes in a 36 weeks baby in his first day of life. The changes included sever blanching of the right toes and the penis, concomitant with sever mottling of the back and anterior abdominal wall mainly on the right side but were not well demarcated. The baby’s clinical condition, transient course of illness and investigations ruled out sepsis or any evidence of thrombosis. Mum turned to have Covid 19 but no evidence it affected the baby, who was discharged on day 6 and is currently 8 months old with no recurrence of such event.
Keywords: Streptobacillus moniliformis; Rat bite fever; Septic arthritis; Osteomyelitis.
Abbreviations: BC: Blood Cultures; CT: Computed Tomography; JF: Joint Fluid; MRI: Magnetic Resonance Image; RBF: Rat Bite Fever; RL: Right Leg; RK: Right Knee; RS: Right Shoulder.
Copy right Statement: Content published in the journal follows Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0). © Batista C (2023)
Journal: Open Journal of Clinical and Medical Case Reports is an international, open access, peer reviewed Journal mainly focused exclusively on the medical and clinical case reports.
Citation: Batista C, Oliveira SR, Jordão S, Rodrigues JC, Abel C, Abreu RC, Neves I. Rat bite fever with multifocal musculoskeletal infection and septic shock. Open J Clin Med Case Rep. 2022; 1973.
Introduction
Rat Bite Fever (RBF) is a zoonosis mainly caused by Streptobacillus moniliformis, a fastidious Gram-negative filamentous rod [1] transmitted by rodent bites or exposure to their fluids [2]. Symptoms such as fever, rash, and migratory polyarthralgia are commonly described [2] and complications may include endocarditis, meningitis, and focal abscesses [3]. Although the infection has a higher incidence in children, adults over 60 years old are more frequently hospitalized [4]. Identification of this microorganism is challenging as it may not grow with laboratory conventional methods [2].
The first line of treatment is Penicillin G and the clinical outcome is usually favorable if antibiotic therapy is started promptly [5]. The mortality rate described can reach up to 7-13% [5].
Case reports of RBF in Europe are scarce [2], however, it is likely that this disease is underdiagnosed due to its nonspecific clinical presentation [6], adequate treatment with short-spectrum and commonly used antibiotics [7] and difficult laboratory identification of Streptobacillus moniliformis [8]. To the best of our knowledge, up to date, only one case of RBF has been reported in Portugal [3].
Case Presentation
We present the case of a 67-year-old man with type 2 diabetes mellitus, arterial hypertension, and degenerative joint disease of the right knee (RK). The patient was admitted to the emergency department with Right Shoulder (RS) and RK arthralgias starting seven days before, with increasing functional limitation. His wife described recent and abrupt onset of confusion, visual hallucinations, and decreased urine output. On physical examination, the patient was conscient, afebrile, with blood pressure of 115/70 mmHg and inflammatory signs on the RS and RK were evident. Blood analysis revealed 20330/μL leukocytes (94% neutrophils), C-reactive protein 600 mg/L, acute kidney injury (creatinine 5.3 mg/dL and urea 144 mg/ mL), and metabolic acidosis (pH 7.30, serum bicarbonate 16.5 mEq/L). Computed tomography (CT) scan showed evidence of septic arthritis of the RK and right subscapular septic bursitis. Blood Cultures (BC) and Joint Fluid (JF) were immediately collected, and the patient started empiric therapy with ceftriaxone 2 g daily. RK arthroscopic lavage and debridement were performed. Within the first 24 hours, the patient developed septic shock and was admitted to the Intensive Care Unit. Due to severe clinical worsening and observation of Gram-negative rods in the Gram stain of the JF, antibiotic therapy was switched to meropenem 2 g every 8 hours.
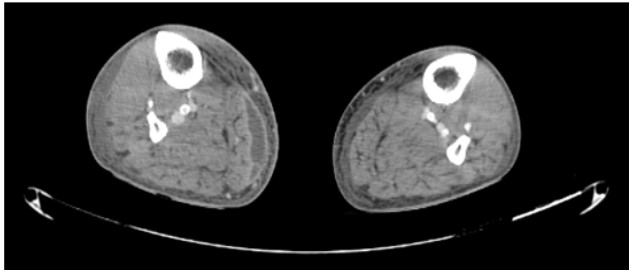
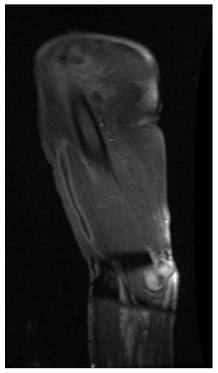
One week later, the patient recovered kidney function, and resolution of cardiovascular dysfunction occurred, enabling the cessation of vasopressor support, but progression with inflammatory signs in the entire right arm and Right Leg (RL) was noticed. CT scan revealed significant periarticular edema on the RK, soft tissues marked swelling and a 6 x 1.5 cm collection in the middle third of the RL (Figure 1). Magnetic resonance image (MRI) identified a 15 x 6 x 1.5 cm collection in the biceps brachii muscle subfascial plane (Figure 2) and an elongated set of collections, measuring up to 2 cm, involving almost the entire lateral longitudinal axis of the arm.
New surgical debridement and source control were performed and in the following weeks four other surgical interventions were required. Additionally, RK subchondral osteomyelitis developed later.
BC initially drawn were negative and the transesophageal echocardiogram showed no signs of endocarditis. Thoracic-abdominal-pelvic and spine CT scan didn’t reveal other infection foci.
The Gram-negative rod of the JF couldn’t be identified by the phenotypic methods (MALDI-TOF and VITEK 2) available in our laboratory. However, the antimicrobial susceptibility testing confirmed sensibility to penicillin, and antibiotic therapy was changed to ampicillin 2 g every 4 hours. On the 29th day of hospitalization, Streptobacillus moniliformis was identified by PCR and sequencing of the 16S rRNA by the national reference laboratory.
After neurological recovery, the patient recalled being bitten by a rat on a finger a few days before the onset of symptoms.
The patient had a good clinical outcome, being discharged after 4 months of hospitalization and antibiotic therapy but remained with joint sequelae and limited mobility of the RS and RK.
Discussion/Conclusion
This clinical case report demonstrates that RBF can have a severe presentation with quick deterioration and risk of death. The rapid initiation of antibiotic therapy combined with surgical interventions for debridement and drainage were crucial for disease control, although motor sequelae remained. In the absence of complications, the recommended treatment duration is 7-14 days [5], however, this clinical case highlights the need for a considerably longer treatment in more complicated scenarios. The patient presented with septic arthritis of the knee, which is the most affected joint in this disease [9]. The presence of degenerative joint disease in the knee most likely increased the risk of developing septic arthritis.
Because of the diverse and non-specific clinical manifestations, the diagnosis was challenging, and it was only established after 16S rRNA sequencing. As this microorganism requires specific culture conditions [2], not available in every laboratory, despite the negative result of BC, bacteremia cannot be excluded [2].
A history of rat exposure should alert to the possibility of RBF and the beginning of prompt and effective treatment for this disease shouldn’t be delayed, avoiding complications and death.
References
- Matthews C, Ausman S. Rat-bite fever: Taking the bite out of a textbook case of Streptobacillus moniliformis blood stream infection. IDCases. 2021; 25: e01199.
- Kämmerer T, Lesmeister T, Wollenberg A, French LE, Strobel E, Reinholz M. Rat bite fever, a diagnostic challenge: case report and review of 29 cases. J Deutsche Derma Gesell. 2021; 19(9): 1283-1287.
- Pena E, Jordão S, Simões MJ, Oleastro M, Neves I. A rare cause of vertebral osteomyelitis: the first case report of rat-bite fever in Portugal. Rev Soc Bras Med Trop. 2020; 53: e20190328.
- Kache PA, Person MK, Seeman SM, McQuiston JR, McCollum J, Traxler RM. Rat-bite fever in the United States: an analysis using multiple national data sources, 2001–2015. Open Forum Infect Dis. 2020; 7(6): ofaa197.
- Zhang WW, Hu YB, He GX, Zhou Y, Hong L, Ding JG. Rat bite fever caused by Streptobacillus moniliformis infection in a chinese patient. BMC Infect Dis. 2019; 19:637.
- Julius RS, Brettschneider H, Chimimba CT, Bastos ADS. Prevalence and diversity of the Streptobacillus rat-bite fever agent, in three invasive, commensal Rattus species from South Africa. Yale J Biol Med. 2021; 94:217-226.
- Khatib MY, Elshafei MS, Mutkule DP, Shabana AM, Chengamaraju D, Nashwan AJ. Rat bite fever: the first case report from Qatar. Am J Case Rep. 2020; 21: e925647.
- Winther M, Jensen HS, Tarpgaard IH, Nielsen HL. Case report: a fatal case of aortic and mitral valve endocarditis caused by Streptobacillus moniliformis. Eur Heart J Case Rep. 2020; 4: 1-6.
- Wang TKF, Wong, SSY.Streptobacillus moniliformis septic arthritis: a clinical entity distinctfrom rat-bite fever?BMC Infect Dis. 2007; 7: 56.