Open Access, Volume 9
Psychological concern among ortho trauma patients: A narrative review
Keerthi Mohanan; Monika Thakur*
AIIMS Patna, NIMHANS Bengaluru, India.
Monika Thakur
AIIMS Patna, NIMHANS Bengaluru, India.
Email: thakurmonika.1793@gmail.com
Received : November 22, 2022
Accepted : January 04, 2023
Published : January 10, 2023,
Archived : www.jclinmedcasereports.com
Abstract
Injury pertaining to musculoskeletal system might be unexpected to the victim both physically and mentally. Injured person might be unprepared to be bombarded with sudden hospital visit, painful procedures and dependence on others. Presence of psychiatric illness might just aggravate the anxiety symptoms and make the prognosis poor. Psychological concerns could be related to emergency admission, initial detailed diagnostic procedures to be undergone, high severity pain, dependency on relatives or hospital staff for doing the basic things. They might start using unhealthy defence mechanism like denial, regression, avoidance just to escape the pain of ortho-trauma. Treatment protocol needs inclusion of psychological issues right from admission to rehabilitation in a team effort.
Keywords: Orthopaedic trauma; Inpatient admission; Psychological issues.
Copy right Statement: Content published in the journal follows Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0). © Thakur M (2023)
Journal: Open Journal of Clinical and Medical Case Reports is an international, open access, peer reviewed Journal mainly focused exclusively on the medical and clinical case reports.
Citation: Mohanan K, Thakur M. Psychological concern among ortho trauma patients: A narrative review. Open J Clin Med Case Rep. 2023; 1961.
Introduction
Orthopaedic trauma is defined as a severe injury to part of the musculoskeletal system such as bones, joints, or ligaments [1]. Road traffic accidents is most common reason of Orthopaedic trauma, other reasons which can attribute to such trauma are industrial injuries, accidents fall and slip [2,3,]. Globally an estimated 103 million people died due to Road traffic accident and around 78.2 million are injured [4]. Worldwide orthopaedic traumatic injuries accounts for accounting for 16% of total burden of the disease [5]. Such trauma not only results in physical effect but also range of other negative health outcomes including mental health problems [6]. Psychiatric disorder and emotional upset are reported to be 3-5% higher among these patients and may continue to persist for a longer duration even after when physical health is restored [7]. Survivors commonly experience post-traumatic stress syndrome, depression, and anxiety, all of which interfere with functional gains and quality of life [6]. Depression and anxiety are the most common disorders occurring in these patients [8,9]. The prevalence of psychological issues is determined by various factors like severity of the injury, time of assessment of psychiatric morbidities and tools used to assess such disorder and other underlying factors such as family support, family responsibilities, financial resources [6,7,9]. This topic highlights the presence of psychological issues among orthopaedic trauma patients and which necessitate the evaluation of such persons and appropriate treatment can be given to alleviate the suffering of such persons.
Table 1: Prevalence of psychological disorder among ortho injury patients.
| 1 | Author and year | Purpose | Research design | Sample characteristics | Sample size /mean age (year) | Results |
|---|---|---|---|---|---|---|
| 2 | Sharma A, CM GD. Study of depressive and anxiety symptoms in patients with orthopaedic trauma. Indian Journal of Orthopaedics. 2016;2(4):393-5. | To identify depressive and anxiety symptoms in post-traumatic patients | Cross sectional study | Post traumatic orthopaedic patients | 108/ 41.9 | 26% of patients in acute duration of orthopaedic trauma i.e., within 45 days of injury had moderate – severe anxiety symptoms and 36% of the patients had moderate – severe depressive symptoms and 8% had both. |
| 3 | Kumar, S., Verma, V., Kushwaha, U., Calvello Hynes, E. J., Arya, A., & Agarwal, A. (2019). Prevalence and association of depression in in-patient orthopaedic trauma patients: A single centre study in India. Journal of Clinical Orthopaedics and Trauma. doi:10.1016/j.jcot.2019.12.010. | To identify the prevalence and identify factors associated with depression in indoor Orthopaedic trauma patients | prospective cohort study | Indoor Orthopaedic trauma patients | 190/33.8 | Frequency of depressive symptoms (HADS>8) was 42.63% among orthopaedic admitted patient. |
| 4 | Malik P, Garg R, Sidhu S, Sharma KC, Gulia AD. Psychiatric morbidity in post traumatic orthopedically handicapped patients. Delhi Psychiatry Journal. 2012 Apr;15(1):130-5. | to find out the prevalence of psychiatric disorders and factors affecting these disorders in post traumatic orthopedically handicapped patients | cross-sectional study | post traumatic orthopedically handicapped inpatients and outpatients | 71/33.29 | (67.6%) had psychiatric symptoms with depressive disorder (38%),PTSD (26.8%). Remaining patients had phobic anxiety disorder (15.5%), adjustment disorder (14%), somatoform disorder (12.7%), and acute stress reaction (4.2%) |
| 5 | Jain R, Rishi R, Sharma B, Kiyawat V. Role of depression and its associating factors in indoor orthopaedic patients. Asian Journal of Medical Sciences. 2015 Jun 16;6(6):70-6. | to investigate the role, prevalence and associating factors of depression disorder in orthopaedic inpatients | cross-sectional study | orthopaedic inpatients | 426/34.17 | Depressive disorder was identified in 87.6% indoor patients significantly (p<0.001) influenced female more than male. |
Causal factors triggering psychological issues
Psychological aspect is one of the neglected or willingly ignored issues among trauma patients. History or presence of psychiatric disorder among trauma victims might cause either delay in approaching treatment, increased risk for trauma, fear and issues regarding healing or body disfigurement might cause altered or poor prognosis [10].
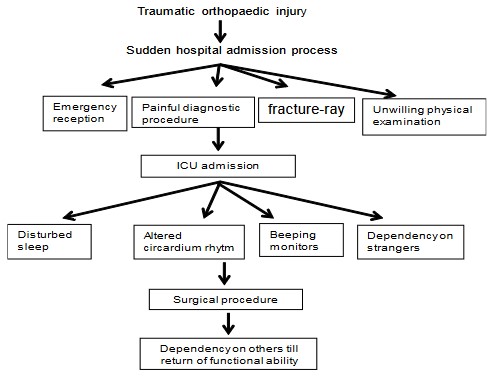
Psychological stress is associated with many factors associated with trauma which could include various components like pattern of trauma, either trauma was sudden or acute, bodily part affected and its importance in one’s daily living and current life social issues being faced by the patient. Trauma patient has to face some unexpected events post injury like experiencing painful trauma, ambulance transport, and transfer from primary health care centre to advanced settings or tertiary care, long waiting for admission procedure, undergoing certain surgical procedures, intensive care admission. The trauma experiencing client is horrified with the pain and unable to adjust to new environment and involvement in all the procedure requiring active participation from him. Admission process involves sudden body exposure for physical examination, unending intravenous puncture and sampling collection for impending surgical procedure that is expected. Then comes investigations like X-ray without any anaesthesia and the technician yelling for correct placement but pain grasped patient starts showing guarded behaviour by that duration after injury [11].
Pain perceived post trauma could be severe in nature and with delay in management of sharp pric-king pain could lead to exaggerated symptoms of anxiety, hostility and sleep disturbances. Sudden feeling of helplessness and being overly dependent on others for basic things might be overwhelming for trauma patients with focussing on pain perception for most part of the day. High frequency of psychological symptoms like anxiety, depression and PTSD has been reported among patients with injury related chronic pain [11,12].
Highly noisy hospital environment with continuous buzzing of machinery sounds like infusion pump beeps, ventilator beeps, monitors further frighten traumatized patient. They lack frame of reference. Limited verbal communication with near and dear one, inability to express ones thought in healthcare professional’s presence lead to emotional distress. Sensory deprivation could be result of closed environment, continuous repetitious hospital routine like constant vital monitoring, medication administration, round the clock healthcare rounds. Patients become less oriented to time and place. A six month follow up study among ICU survivors of traumatic injury found prevalence risk for of PTSD as high as 21% and some of the ICU conditions like coma time, mechanical ventilation, sedation, use of sedatives like benzodiazepine, pain relieving medication, and symptoms of acute stress , worrying about reaching deathbed , feeling completely helpless or completely dependent on others and powerless in relation to the accident and/or ICU correlated significantly with PTSD symptoms [11,13].
Psychological issues
Psychological reactions shown by trauma patients might be an eye view of various coping mechanism being in collation with defence mechanism. Previous studies point that victims blaming others for events leading to trauma have shown poor outcome related to functional aspect, health outcomes and returning to work [14]. Traumatic event continues to run in flashback and patient claim’s self-blame how it could have been averted, if at that particular moment he or she might have been more careful. The scar injury continues to be a persistent reminder of the traumatic event especially injuries affecting functional changes [15]. Disappointment regarding inability to attend many of family gathering because of trauma injury and ashamed feeling of body image due to trauma disfigurement or surgery marks. Prolonged grief could be seen along with feeling of loss of control, loss of certain body image, loss of social connection or loss of financial stability. The overnight or within fraction of seconds changes make them unable to accommodate to these changes especially changes involving sensory perceptions like phantom limb sensation or pain [16].
Sleep deprivation is one of the major causes of emotional up-down among trauma patient. Natural circadian rhythm is disturbed pertaining to round the clock hospital lightings, noisy monitors and ineffective management of pain during various surgical procedures. Identification of hospital environment as a strange and unfamiliar new area creates unnecessary thoughts, doubts and overthinking continues regarding poorest prognosis gives mind less time for healthy sleep. It has been reported among inpatient traumatic orthopaedic patient that nearly 86% of the patient’s had sleep disturbances and sleep disturbance was found to be associated with bodily pain vitality and mental health issues cited by these patients [17].
Presence of psychiatric illness in hospitalized patients with orthopaedic injuries and that psychiatric comorbidity is correlated with higher prevalence of surgical complications, longer hospital stay and higher in hospital mortality. It has been witnessed from the previous researches that, low-income patients with psychiatric illness remain in acute hospital care twice as long as the conventionally insured patients [18]. Immune modulation could be one of the reasons for higher post-operative infection rates among patients with psychiatric illness. Cytokines like IL B, IL-6 and TNFα can trigger inflammatory response initiating psychological stress. Depression induces immune dysfunction by acting on pro-inflammatory cytokines [19].
Approaches to addess psychological issues
Once the physical ailment is corrected and patient is stabilized attention should be given to psychological impact of trauma. Psychological interventions are required at various stages of treatment [20]. Literature about orthopaedic injuries suggest the importance of addressing the psychological issue along with physical disability in order to improve quality of life among ortho-injury patients [10]. It is essential to envisage the adverse use of mental mechanism like denial, anger and other Greif reaction. In early phase of injury patients may not accept the accident (Denial) which somewhere may help in reducing development of depression and anxiety, so use of defence mechanism like denial should not be abruptly removed. In this stage patient must be encouraged to communicate fear, worries and thoughts of self-destruction and guilt [11]. Management of the anger is essential as this may lead to self-harm or aggression .Past studies suggested the association of pain with anger [21]. Henceforth managing pain will be helpful in reducing the anger and associated reactions [22]. Grief is a gradual process which will subside with time, adequate measure like family support, emotional and psychological support must be given for healthier come out from this situation.
Patient who will undergo surgical procedure intervention are required at various stages i.e. Preoperatively, postoperatively and at the time of rehabilitation.
Preoperative psychological care is required for addressing emotional needs prior to performance of any surgical intervention [23]. Patient’s suffering from any psychological issues (such as depression or grieving), are at higher risk of having less functional improvement after orthopaedic surgery. Research studies have suggested the effectiveness of educational intervention preoperatively to improve emotional health [24-26].
Successful postoperative care may require different care pathways with different levels of support, depending on the patient’s preoperative psychological health [27]. Such pathways may involve teams of clinicians, including physical therapists, behavioural psychologists, and other support professionals. More research is needed to define perioperative interventions that need to be adopted by health care personnel dealing ortho injury patients that will simultaneously support the physical and mental health of the patients to ensure optimal functional gain after successful surgery. Finding practical financial and operational models to follow tailored pathways of care will be much suitable.
Non-judgmental social support provided to patients by nonfamily member is important to the patient’s positive outlook while he or she is in the hospital [8]. Physical injury resulting due to orthopaedic trauma once corrected requires physical rehabilitation to achieve optimum level of rehabilitation. But in various settings from long time, much focus was given to physical rehabilitation to correct the functional deficit whereas psychological impact of the illness were not assumed or ignored [28]. It is detrimental from previous studies that psychiatric comorbidity will be able to determine the prognosis of the patients and acute and chronic recovery [29-31]. Early recognition and assessment of patients with distress can help health care team members provide the needful resources and support for reduction of distress. Holistic approach needs to be adopted for quality care.
Several interventions and strategies that can help trauma patients enhance their short-term recovery include holistic approaches, brief counselling sessions, relaxation techniques, interventions from positive psychology use of adaptive coping skills, mindfulness, peer visitation, and educational resources [32-34]. Study conducted on effect of stress inoculation training (cognitive behavioural interventions) resulted in reduction of pain and anxiety among orthopaedic injury patients [35]. The long-term physical and mental health of the trauma survivor can be enhanced by strategies that connect the survivor to a network of people with similar experiences or injuries, facilitate support groups, and social support networking. Rehabilitation specialists need to pay much attention toward psychological issue which can help optimize patient outcomes and quality of life by participating in and advocating these strategies [8].
Conclusion
In the current review it is observed that psychological issues among orthopaedic trauma patients are prevalent with depression and anxiety as most common psychiatric morbidly. Routine assessment and appropriate interventions can be used to address the psychological issues arisen due to orthopaedic trauma. Special attention need to be paid to those who are at higher risk such as females, amputated patients, patients with severe pain and fracture and other associated medical comorbidities. Further researches are required to find the relationship between severity of psychiatric disorders and factors such as comorbid medical illness and amputation. Research should evaluate cost-effective strategies that need to be identified to accomplish this goal.
References
- Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bulletin of the world health organization. 2003; 81: 646-656.
- Huda N, Gupta P, Pant A, Iqbal A, Julfiqar M, et al. Pattern of Orthopaedic injuries among patients attending the emergency department in a tertiary care hospital–An analytical study. Acta medica international. 2014; 1: 10.
- Hanche-Olsen TP, Alemu L, Viste A, Wisborg T, Hansen KS. Trauma care in Africa: a status report from Botswana, guided by the World Health Organization’s “Guidelines for Essential Trauma Care”. World journal of surgery. 2012; 36: 2371-2383.
- Global Road Safety Facility. Transport for health: the global burden of disease from motorized road transport.
- World Health Organization. Guidelines for essential trauma care. World Health Organization; 2004.
- Ponsford J, Hill B, Karamitsios M, Bahar-Fuchs A. Factors influencing outcome after orthopedic trauma. Journal of Trauma and Acute Care Surgery. 2008; 64: 1001-1019.
- Kuhn WF, Bell RA, Netscher RE, Seligson D, Kuhn SJ. Psychiatric assessment of leg fracture patients: A pilot study. The International Journal of Psychiatry in Medicine. 1990; 19: 145-154.
- Vincent HK, Horodyski M, Vincent KR, Brisbane ST, Sadasivan KK. Psychological distress after orthopedic trauma: prevalence in patients and implications for rehabilitation. PM&R. 2015; 7: 978-989.
- Srahbzu M, Yigizaw N, Fanta T, Assefa D, Tirfeneh E. Prevalence of depression and anxiety and associated factors among patients visiting orthopedic outpatient clinic at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia, 2017. J Psychiatry. 2018; 21: 2.
- Bhandari M, Busse JW, Hanson BP, Leece P, Ayeni OR, et al. Psychological distress and quality of life after orthopedic trauma: an observational study. Canadian Journal of Surgery. 2008; 51: 15.
- Mohta M, Sethi AK, Tyagi A, Mohta A. Psychological care in trauma patients. Injury. 2003; 34: 17-25.
- Stålnacke BM. Psychological symptoms in patients with injury-related chronic pain. ISRN psychiatry. 2012; 2012.
- Ratzer M, Brink O, Knudsen L, Elklit A. Posttraumatic stress in intensive care unit survivors–a prospective study. Health Psychology and Behavioral Medicine: an Open Access Journal. 2014; 2: 882-898.
- Gabbe BJ, Simpson PM, Cameron PA, Ekegren CL, Edwards ER, et al. Association between perception of fault for the crash and function, return to work and health status 1 year after road traffic injury: a registry-based cohort study. BMJ open. 2015; 5: e009907.
- Belzer KL. Coping with the Emotional Impact of Orthopedic Surgery. 2008.
- Bolton MA, Lobben I, Stern TA. The impact of body image on patient care. Primary care companion to the Journal of clinical psychiatry. 2010; 12.
- Swann MC, Batty M, Hu G, Mitchell T, Box H, Starr A. Sleep disturbance in orthopaedic trauma patients. Journal of orthopaedic trauma. 2018; 32: 500-504.
- Schwartz S, Bazargan-Hejazi S, Pan D, Ruiz D, Shirazi A, Washington E. Association of psychiatric diagnostic conditions with hospital care outcomes of patients with orthopedic injuries. The Permanente journal. 2018; 22.
- Dedeogullari E, Paholpak P, Barkoh K, Lucas J, Lee L, et al. Effect of mental health on post-operative infection rates following cervical spine fusion procedures. Journal of orthopaedics. 2017; 14: 501-506.
- Schnaper N, Cowley RA. Overview: psychiatric sequelae to multiple trauma. The American journal of psychiatry. 1976.
- Castillo RC, Archer KR, Newcomb AB, Wegener ST. Pain and psychological distress following orthopedic trauma: a call for collaborative models of care. Techniques in Orthopaedics. 2016; 31: 228-234.
- Gustafsson M, Ekholm J, Ohman A. From shame to respect: musculoskeletal pain patients’ experience of a rehabilitation programme, a qualitative study. Journal of rehabilitation medicine. 2004; 36: 97-103.
- Robleda G, Sillero-Sillero A, Puig T, Gich I, Baños JE. Influence of preoperative emotional state on postoperative pain following orthopedic and trauma surgery. Revista latino-americana de enfermagem. 2014; 22: 785-791.
- Ayers DC, Franklin PD, Ring DC. The role of emotional health in functional outcomes after orthopaedic surgery: extending the biopsychosocial model to orthopaedics: AOA critical issues. The Journal of bone and joint surgery. 2013; 95.
- Paulsen MG, Dowsey MM, Castle D, Choong PF. Preoperative psychological distress and functional outcome after knee replacement. ANZ journal of surgery. 2011; 81: 681-687.
- Wong EM, Chan SW, Chair SY. Effectiveness of an educational intervention on levels of pain, anxiety and self-efficacy for patients with musculoskeletal trauma. Journal of Advanced Nursing. 2010; 66: 1120-1131.
- Nickinson RS, Board TN, Kay PR. Post-operative anxiety and depression levels in orthopaedic surgery: a study of 56 patients undergoing hip or knee arthroplasty. Journal of evaluation in clinical practice. 2009; 15: 307-310.
- Soberg HL, Bautz-Holter E, Roise O, Finset A. Long-term multidimensional functional consequences of severe multiple injuries two years after trauma: a prospective longitudinal cohort study. Journal of Trauma and Acute Care Surgery. 2007; 62: 461-470.
- Holbrook TL, Anderson JP, Sieber WJ, Browner D, Hoyt DB. Outcome after major trauma: discharge and 6-month follow-up results from the Trauma Recovery Project. Journal of Trauma and Acute Care Surgery. 1998; 45: 315-324.
- Helmerhorst GT, Vranceanu AM, Vrahas M, Smith M, Ring D. Risk factors for continued opioid use one to two months after surgery for musculoskeletal trauma. JBJS. 2014; 96: 495-499.
- Nhac-Vu HT, Hours M, Chossegros L, Charnay P, Tardy H, et al. Prognosis of outcome in adult survivors of road accidents in France: one-year follow-Up in the ESPARR cohort. Traffic injury prevention. 2014; 15: 138-147.
- Louw A, Diener I, Butler DS, Puentedura EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Archives of physical medicine and rehabilitation. 2011; 92: 2041-2056.
- Cherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, et al. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial. Jama. 2016 Mar 22; 315: 1240-1249.
- Kearney DJ, Simpson TL. Broadening the approach to posttraumatic stress disorder and the consequences of trauma. Jama. 2015; 314: 453-455.
- Ross MJ, Berger RS. Effects of stress inoculation training on athletes’ postsurgical pain and rehabilitation after orthopedic injury. Journal of consulting and clinical psychology. 1996; 64: 406.